Gut Feeling
Learn more about your ad choices. Visit podcastchoices.com/adchoices
Press play and read along
Transcript
Speaker 1 Enemy forces are reported to be armed with stolen small arms, including M16 and AK-47 rifles.
Speaker 1 To help maintain security and peace in the area of operations, your mission will involve manning checkpoints to interrupt the movement of enemy forces. So it looks like you're in a city here.
Speaker 2 And right now, I'm trying to figure out if the individual walking towards me is a friend or a foe based on his camouflage patterns. I'm going to call that a foe, so I'm going to shoot.
Speaker 1 I got it right.
Speaker 3
That's right. Gastropod has become a military gaming show.
This week, Cynthia shoots the enemy and sometimes her friends, too.
Speaker 1 Watch out, world. All my friends should definitely be concerned because I am not so great with a gun, even if it's a virtual one.
Speaker 1 But luckily, I was not the one who really needed to worry about whether the person advancing was friend or or foe. I was watching the future of the U.S.
Speaker 1 Army's plans to tweak warfighter guts so that the soldiers make better life and death decisions.
Speaker 3 You might be thinking, well, I have no plans to shoot anyone right now, and honestly, for that, we're grateful. But this research goes well beyond a battlefield application.
Speaker 3 If manipulating our gut microbiomes can really change how we think and feel, that's news we can all use.
Speaker 1 As you listeners already know, gut microbes are something we love here at Gastropod, the podcast that looks at food through the lens of science and history. I'm Cynthia Graeber.
Speaker 3
And I'm Nicola Twilley. And first of all, a PSA.
For your own health, please don't drink every time we say microbe this episode.
Speaker 1 Because this episode, we're diving into our guts to meet our gut microbes to find out how they're connected to our brains. Will gut microbes be the next mental health therapeutic breakthrough?
Speaker 3 It's a story that involves all our favorite things. fecal transplants, fermented foods, and lots and lots of stressful situations.
Speaker 1 Just another day here at Gastropod. Today's episode is supported in part by the Burroughs Welcome Fund in support of our coverage of biomedical research and by the Alfred P.
Speaker 1 Sloan Foundation for the Public Understanding of Science, Technology, and Economics. Gastropod is part of the Vox Media Podcast Network in partnership with Eater.
Speaker 5
Support for this show comes from Pure Leaf Iced Tea. When you find yourself in the afternoon slump, you need the right thing to make you bounce back.
You need Pure Leaf Iced Tea.
Speaker 5 It's real brewed brewed tea made in a variety of bold flavors with just the right amount of naturally occurring caffeine.
Speaker 5
You're left feeling refreshed and revitalized, so you can be ready to take on what's next. The next time you need to hit the reset button, grab a Pure Leaf Iced Tea.
Time for a tea break?
Speaker 5 Time for a Pure Leaf.
Speaker 4 Thumbtack presents Project Paralysis.
Speaker 6 I was cornered.
Speaker 4 Sweat gathered above my furrowed brow and my mind was racing. I wondered who would be left left standing when the droplets fell, me or the clawed sink.
Speaker 4 Drain cleaner and pipe snake clenched in my weary fist, I stepped toward the sink and then, wait, why am I stressing?
Speaker 3 I have thumbtack.
Speaker 4 I can easily search for a top-rated plumber in the Bay Area, read reviews, and compare prices, all on the app.
Speaker 3 Thumbtack knows homes. Download the app today.
Speaker 8 Okay, let's talk about this because I think it's super, super powerful. There is something called the gut-brain connection.
Speaker 8 And pretty much what it says is that inflammation in your gut can really worsen symptoms of anxiety and depression and other mental illnesses.
Speaker 8 I sound like a broken record but adding in a probiotic literally changed my life.
Speaker 9 I used to have crippling anxiety panic attacks constantly and now I don't have them anymore and the only thing I changed was the food I was eating.
Speaker 3 TikTok influencers are not people you should be taking any medical advice from ever but there's a lot of hype out there about this gut-brain connection and the idea that you can change your mental health by changing what you eat.
Speaker 1 This episode, this is what we're getting to the bottom of. Is it actually true?
Speaker 10 Depression, anxiety, cognitive disorders, sleep disorders, and the fifth category I will call really the area of focus and attention.
Speaker 3 This is Uma Naidu. She's a nutritional psychiatrist at Harvard and the author of This is Your Brain on Food.
Speaker 3 And her list is just a few of the mental health conditions that it seems can likely be treated by tweaking your gut microbiome.
Speaker 1 As we just said, we of course are obsessed with microbes. And so yes, we've talked about the gut microbiome before.
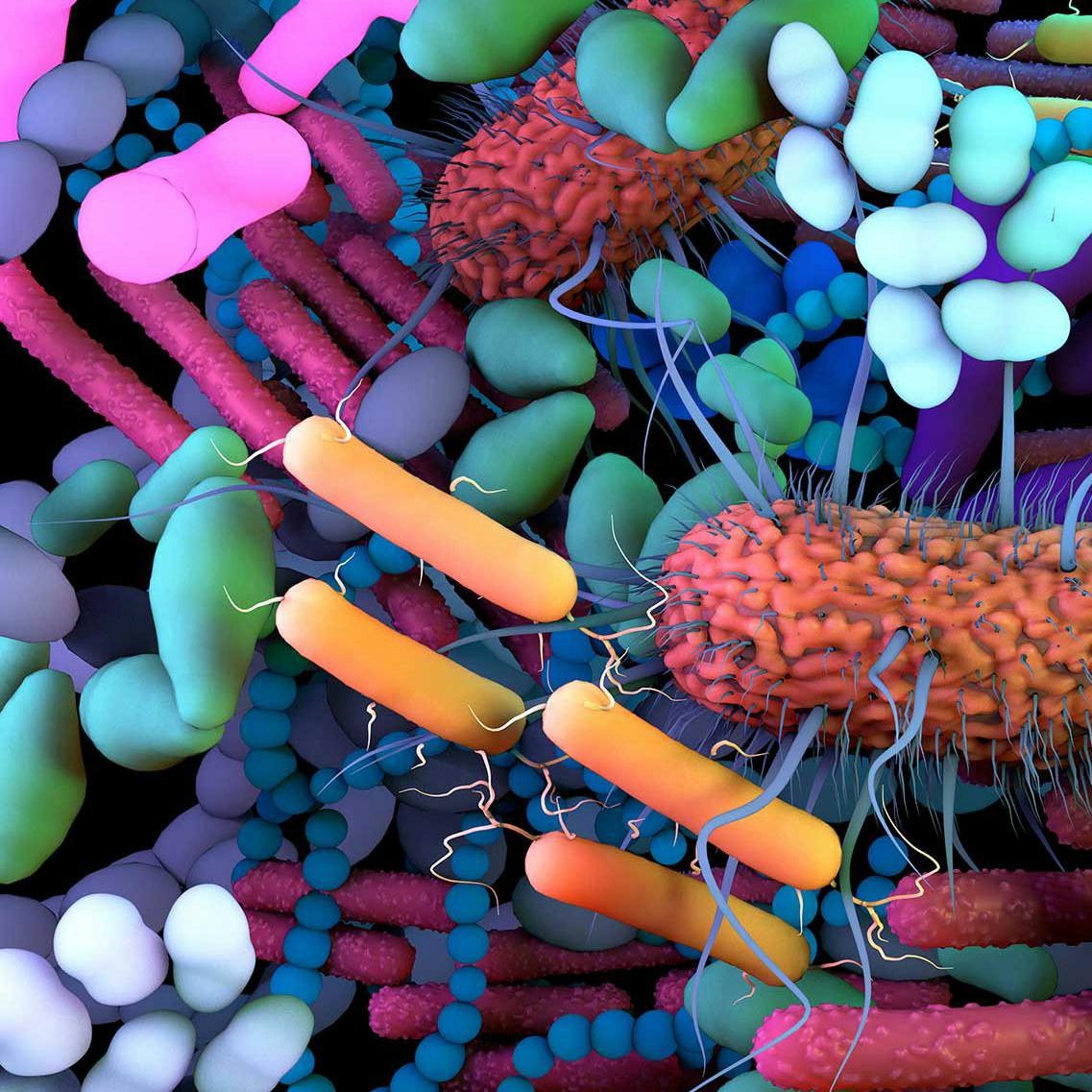
Speaker 1 But if you don't remember the particulars, there are about 100 trillion bacteria in your gut, and they belong to hundreds of different species.
Speaker 1 They feed on what you eat, they break it down for you, they create important new compounds out of that food.
Speaker 1 Basically, your gut microbiome is both incredibly important and kind of wildly fascinating, especially for this episode and how it connects to your brain.
Speaker 3 If you're thinking, well, I don't know about this.
Speaker 3 Last I heard, if you're depressed or anxious or whatever, your mental health professional is probably going to prescribe therapy or drugs rather than try to change your gut microbes.
Speaker 3 Well, that's because this research is all pretty new.
Speaker 10 The science of the gut microbiome, that gut-brain connection that we talk about, is really only a couple of decades old.
Speaker 3 When Uma trained as a psychiatrist, no one even mentioned the gut microbiome. The science of the gut and the science of the brain were two separate things, and that was that.
Speaker 11 You know, if you study neuroscience, you study from the neck upwards, more or less. And when you study the gut, you study gut physiology and you study it from a gastroenterology perspective.
Speaker 11 And one of the things of our modern medicine is that we compartmentalize the body. And so we get very discipline-specific.
Speaker 1 John Cryan is a professor of anatomy and neuroscience at University College Cork, and he's one of the rock stars in the field of the gut-brain connection.
Speaker 3 Find a small enough niche, and you too can be a rock star. But seriously, John Cryan and his colleagues more or less founded the gut microbiome mental health field.
Speaker 1 John caught the first glimpse of what would become really his life's work back in 2004 when he read a paper in the Journal of Physiology.
Speaker 11 So, not a glamour journal, from a group in Japan, which had shown that in germ-free animals, these are animals that grow up without microbes, that they have an exaggerated stress response.
Speaker 11 So, they predicted, although it wasn't really well talked talked about at the time, that the microbes in the gut were regulating the stress response.
Speaker 3 Which was a novel and very intriguing idea.
Speaker 3 In John's lab, they started out looking at stressed mice and they noticed a couple of really interesting things in mice that had been stressed while they were still babies.
Speaker 3 First of all, as adults they behaved differently from mice that hadn't had that early stress.
Speaker 3 And then also the microbes living in their guts were different from the ones found in mice that had had a chill lifestyle as babies.
Speaker 11 And that's really got me kind of hooked because we kind of were like, could be down to many things, but what if it's something is there about how stress and the microbiome are interacting?
Speaker 1 That was interesting enough to make John keep looking to try to isolate the microbes he thought might be affecting the stress response.
Speaker 11 And then in 2011, we published a paper showing that could you then target the microbes in your gut with a specific bacteria and could you alleviate the effects of stress in animals?
Speaker 3 And it turns out that yes, you could.
Speaker 3 John and his colleagues showed that you could feed your mice some specific microbes, microbes that are typically found in yogurt, and that intervention alone was enough to ramp down their stress levels.
Speaker 1 How did they figure out if the mice were less stressed? Well, the mice were put in water in tall cylinders that they couldn't crawl out of. They had to keep paddling.
Speaker 1 The ones who gave up quickly and just floated, they're seen as more stressed. The official term is behavioral despair.
Speaker 1 The ones who had been fed those yogurt microbes and felt calmer kept swimming longer.
Speaker 3 Do not worry, all of the mice, whether they were swimmers or despairers, they were all rescued unharmed.
Speaker 11 And so we did these experiments, and that was kind of our eureka moment to kind of say, okay, psychobiotics.
Speaker 1 Before we at Gastropod started looking into this, I had never heard of a psychobiotic before. What in the world? Aha.
Speaker 11 So psychobiotic is a word that we coined here in Cork, my colleague Ted Dine and I. And it's a word that has evolved in its meaning.
Speaker 11 And right now, I would say that a psychobiotic is an intervention that targets the microbiome for mental health benefit.
Speaker 3 So John's first Eureka moment, feeding microbes to his mice to keep them from giving in to despair, him and Ted coming up with this fabulous new word psychobiotic.
Speaker 3 This is all happening around the same time in 2011. And then there was another breakthrough.
Speaker 11 We showed back then, around the same time in 2011, but also groups at the Karlinska in Sweden and at Blackmaster in Canada, all at the same time in different strains of mice, in different behavioral tasks, we all showed that these mice, if they grow up without bacteria, in addition to their stress response being changed, their brains don't develop normally.
Speaker 3 The baby mice without any bacteria in their guts, there's a couple of regions in their brains that end up pretty different from mice who grew up with gut microbes.
Speaker 3 So, for example, there's a region in mouse and human brains called the amygdala, which is linked to emotions like fear and anxiety.
Speaker 3 In the baby mice without gut microbes, the neurons in their developing amygdala end up making different connections.
Speaker 1 The microbes in the mouse guts also seem to affect the insulation around parts of the brain that transmit electrical signals. How this all works isn't totally clear.
Speaker 1 There seems to be a way in which chemicals that microbes make are helping tell the brain how to develop, but that still has to be worked out. That said, it's a really striking scientific result.
Speaker 11 And so that was also a second Eureka moment in terms of where we could realize that there is a clear relationship between the composition of microbes in your gut and how your brain functions.
Speaker 3 This all sounds completely bizarre. Like the actual shape and connections of your brain are changed by the microbes in your gut until you remember that we evolved side by side with these microbes.
Speaker 3 They're basically part of us and they always have been.
Speaker 11 We need to take things in an evolutionary context and remember that we are living in a microbial world.
Speaker 1 We are living in a microbial world and I am a microbial girl.
Speaker 1 Sorry about that.
Speaker 3 We couldn't resist.
Speaker 1 Back to microbes and the brain.
Speaker 11 The microbes were here first. So there's never been a time where our brain has existed without microbial signals.
Speaker 11 And we have co-evolved with them and they are our friends with benefits and in particular their brain benefits overall.
Speaker 3 But even though the relationship goes way back, this science is still, like Guma says, really pretty new and exciting.
Speaker 1 Exciting, definitely, but not necessarily totally new. In fact, it started a few thousand years ago.
Speaker 11 Well, everything goes back to Hippocrates. Hippocrates is, well, he's taught to have said that all diseases begin in the gut.
Speaker 12 I think since Greek medicine and Galenic medicine, there was always a strong sense that the emotions and the stomach were somehow connected.
Speaker 12 and that the health of both your mind and the gut were interconnected.
Speaker 3 That second voice is Ian Miller. He's a medical historian at Ulster University in Northern Ireland and the author of a book called A Modern History of the Stomach.
Speaker 3 And he told us that for most of history, all the way through the 1800s, this stomach-brain connection was accepted wisdom in medicine.
Speaker 3 It just seemed like the likeliest explanation for how things worked.
Speaker 12 I think at the time in the 19th century, obviously for much of the century you can't really access the, well, not the living body.
Speaker 12 You can do pathological anatomy, you can dissect bodies once they're dead but it's really hard to really know what's going on inside the body so for me in my opinion one of the reasons why these ideas were so popular was because doctors continued to rely on common sense and and basic things like eating and diets and those kind of things the idea of that brain-stomach connection does make sense when i get super stressed or anxious i often feel like i'm about to throw up others like chandler and friends they get that nauseated feeling when they're excited.
Speaker 2 Man, I'm so excited.
Speaker 10 I'm a vomit.
Speaker 1 Stefani Milan Müller is a postdoc at the Complutense University of Madrid, and she says that Chandler and I aren't alone.
Speaker 13 Even in popular fiction and literature, you often read about things like the butterflies in your stomach.
Speaker 14 I was tried never to be scared of anything. Though I must say, before a big bike event, I do sometimes get nervous, you know.
Speaker 14 If the butterflies in my stomach were
Speaker 14 cows,
Speaker 14 I'd be able to start a
Speaker 14 dairy farm.
Speaker 13 Sometimes, you know, when you're either excited about something, you have that feeling in your gut, or when you're really stressed or anxious, you kind of feel nauseous.
Speaker 13 So there was always this kind of a thing with the gut and feelings.
Speaker 3 In fact, from the late 1700s onward, Ian says that most doctors thought the stomach was the most important organ in the entire body. That it totally governed how you felt in every way.
Speaker 12 So in the 19th century, you get all these references to the stomach as being the great nervous center of the body.
Speaker 12 A lot of these ideas stem from the fact that the stomach is believed to have many, many nerve endings.
Speaker 1 Which scientists have since confirmed that it actually does.
Speaker 1 And the idea at the time was that if the food you ate affected those nerve endings in your stomach, it would also affect your nerves in other parts of your body.
Speaker 12 So, it made sense that if you weren't eating properly and that was affecting the health, the quality of your nerves in your stomach, then your mental health or your emotional well-being could easily decline quite
Speaker 3 In the early 1900s, some doctors actually started prescribing sour milk to treat melancholia. This was basically a kind of early Prozac in the form of kefir.
Speaker 3 There was one British doctor in particular. He worked at the mental hospital whose name ended up becoming the byword for chaos, the Bethlehem,
Speaker 3 better known as Bedlam. And this doctor treated his patients with sour milk and reported a two-thirds success rate.
Speaker 1 Not sure what his controls were, but this was such a hot field at the time that by 1917 in America, there were 30 different supplements on the market that targeted the gut to improve mental health.
Speaker 1 A New York company called Berlin Labs sold an intestifirmin tablet that was marketed as a capsule version of the microbes in sour milk.
Speaker 1 It, quote, attacks the poisons in the gut to quote, promote physical and mental health and provide a truly scientific aid to high efficiency in everyday life.
Speaker 3 Sign me up. Meanwhile, on the other side of the Hudson, a New Jersey doctor was treating mental illness by just removing the gut microbiome altogether, by cutting out his patients' colons.
Speaker 3 He apparently killed 30% of them, but for the ones who lived, he reported an 80% cure rate.
Speaker 1 Again, not sure I'd trust his stats, but the gut was definitely the hottest thing in mental health at the time.
Speaker 3 But also at the time, in the 19 teens and 20s, an obscure former eel biologist known as Sigmund Freud was making a bit of a splash with psychoanalysis.
Speaker 3 And then by 1951, the first antidepressant was invented. It was an antibiotic that seemed to boost serotonin levels in the brain, and it led to a wave of new drugs like Prozac.
Speaker 3 And so the gut just fell out of the picture when it came to mental health.
Speaker 1 These new drugs that became so popular so quickly, they seem to work by mimicking and affecting the levels of what are called neurotransmitters in the brain.
Speaker 1 These are chemicals like serotonin that allow the neurons in the brain to communicate with each other.
Speaker 10 So these chemical neurotransmitters are the ones that that very simply are autophoac when we have different mental health conditions.
Speaker 10 We've studied many of them and we therefore develop medications and pharmaceuticals to adjust those hormone or neurochemical levels. For example, selective serotonin reuptake inhibitors are just that.
Speaker 10 The SSRIs like Prozac, Zolof, Paxil and more adjust those neurochemical levels and help the balance.
Speaker 3 Today, that's mostly how mental health conditions are treated. Therapy and drugs that aim to tweak our neurochemistry directly.
Speaker 3 But what's weird is those chemicals that we're tweaking in our brains, they're found in our guts too.
Speaker 10 So, for example, we often talk about serotonin being the happiness hormone. More than 90 to 95% of serotonin is made in the gut.
Speaker 13 The gut also produces about 50% of the body's dopamine, which is involved in reward and motivation.
Speaker 1 Like many things about this episode, this fact sounds bizarre. But a lot of chemicals and receptors do things in different parts of the body, not just what they're most famous for.
Speaker 1 Some of you might remember that there are umami receptors in human testicles.
Speaker 3 I mean, who could forget? But this is a normal evolutionary efficiency thing in nature.
Speaker 3 The same chemicals and receptors are found all over our bodies, doing different things, and also in different species.
Speaker 3 Serotonin and other chemicals that we call neurotransmitters, they're also found in signaling systems in plants and in bacteria and our brains and our guts.
Speaker 1 In fact, in our guts, serotonin is what tells our colon to contract and squeeze without us noticing in order to move material along for us to poop.
Speaker 1 Maybe this is part of the reason we feel so good after a successful bathroom visit. But on a more serious note, doctors actually prescribe low doses of Prozac to help deal with constipation.
Speaker 3 Prozac isn't serotonin. It just seems to work by stopping serotonin from being absorbed so quickly so that the serotonin can stick around doing its signaling thing for longer.
Speaker 1 The serotonin in our guts is made entirely by microbes. They eat some of the food we eat and they excrete serotonin.
Speaker 1 We do make some of our own serotonin too in our brains, but a much smaller percentage than in our gut.
Speaker 1 As Uma said, an astounding 90 to 95 percent of all the serotonin in our body comes from bacteria in our guts.
Speaker 3
So serotonin is sloshing around in both our brain and our guts. Some is homemade, some is microbe-made.
It's doing its different thing in each place. So far, so good.
Speaker 3 But how are these two separate serotonin situations even connected?
Speaker 10 These two organs, while far apart in the body, arise from the exact same cells in the human embryo.
Speaker 10 They divide up, they form two different organs, but then they remain connected throughout life by the tenth cranial nerve, which is the vagus nerve.
Speaker 10 And I like to call the vagus nerve a two-way text messaging system that's working all the time, sending these chemical messages between the two organs and making changes that way.
Speaker 3 This nerve is one of 12 nerves that originate from the brain, not the spine.
Speaker 3 It's also called the wanderer nerve because it's the longest of those 12 and on its long and windy path it connects the brain to all sorts of different parts of the body.
Speaker 3 the lungs, the spleen, liver, pancreas, heart, and of course the digestive system.
Speaker 1 John was one of the researchers who, about a decade ago, identified the vagus nerve as a potential highway between the gut and the brain for things like serotonin to travel on.
Speaker 1 But he wanted to prove it. So, as you might remember, John and his colleagues had figured out that a specific microbe from yogurt helped mice feel less despair.
Speaker 1 They didn't give up as quickly in that floating test.
Speaker 11 So, we had identified a specific bacteria, a lactobacillus, that when we gave it to mice, they were more chilled out, more relaxed, less stressed, and had changes in their brain.
Speaker 11 And so, we we thought well could the vagus nerve be sending these signals to the brain and so we cut the vagus and all of the effects of this lactobacillus were gone so what this means is that what happens in vagus doesn't just stay in vagus but will actually affect our emotions in in different ways and that is my oldest joke and i apologize for it and i should have apologized in advance that is a gastropod quality dad joke and i am impressed and also a little shocked.
Speaker 3 What this means is that microbial excretions in our gut can actually make us less stressed, which is weird.
Speaker 1
Other researchers have shown similar results. One study showed that giving participants a particular bacteria was kind of like taking an anti-anxiety drug.
That's how much it helped calm people down.
Speaker 3 But this vagus nerve, it's a two-way highway, which means neurotransmitters can go down from the brain to the gut as well as the other way around. And it can be hard to know which came first.
Speaker 3 For example, irritable bowel syndrome is often accompanied by anxiety.
Speaker 1 So the theory is that maybe scientists could treat the bowel symptoms by treating the anxiety.
Speaker 1 They're giving IBS patients cognitive behavioral therapy to ease their anxiety to see if that could help with their guts.
Speaker 3 And some studies have shown that it works.
Speaker 1 But it's not always a positive back and forth. I mentioned that I sometimes feel like I'm about to puke when I'm stressed, and it turns out that mental stress actually changes my gut microbiome.
Speaker 13 So exposure to stress or general emotions can also have an effect on which microbes flourish and the composition of the gut microbiome.
Speaker 13 And by the time you actually have the presentation of anxiety and depression, it's kind of impossible to tease out what came first or what is happening.
Speaker 3 It can be hard to keep a lid on what's happening in vagus or what's zipping up and down the vagus nerve.
Speaker 1 But that direct route is not the only way our gut microbes have to get at our brains.
Speaker 10
The gut itself has a single cell lining. It's a single layer.
it's very delicate, that's why it's easily damaged.
Speaker 10 But it also then interfaces with the circulatory system, which then, through our blood, takes substances and chemicals and all sorts of things all over the body.
Speaker 1 And the chemicals that the microbes living in our gut make can sometimes find ways to squeeze between the cells and the single layer of the gut wall and get into the bloodstream.
Speaker 3 And these chemicals can then have all kinds of effects because it turns out that microbes aren't just excreting neurotransmitters. Some gut microbes make things called cytokines.
Speaker 3 You might have heard of these as part of the body's response to COVID. They're little molecules that trigger immune responses like inflammation.
Speaker 1 And if they leak through the gut's membrane, they can find their way through the blood to the brain, and sometimes they can get past the barrier that protects the brain.
Speaker 13 And have subsequent effects like increasing neuroinflammation, which we know is a big problem in many psychiatric conditions. So a lot of the patients suffer from this
Speaker 13 low-grade systemic inflammation and neuroinflammation.
Speaker 3 So if you combine the vagus nerve and then these leaky barriers between our guts and brains and the bloodstream that connects them, there's at least a couple of clear pathways that chemicals can use to move between our brains and guts.
Speaker 3 So that's the mechanism piece. The exact details are still being teased out, but those seem to be the main pathways for this gut-mental health connection.
Speaker 1 And there's more and more research showing that this does happen and it does have an impact.
Speaker 1 In one study, scientists took gut microbes microbes from feces from a few dozen people with severe depression and from people who didn't have depression.
Speaker 1 They transferred those microbes into rat guts, and the rats who got the depressed fecal transplant got depressed. And that's not all scientists have shown through fecal transplants.
Speaker 10
They transplanted the microbes from patients with schizophrenia into germ-free mice. So the mice didn't have any microbiome.
And over time, those mice developed symptoms of schizophrenia.
Speaker 3 Now, a cynic might say, excuse me, how exactly do you know if a rat is depressed or a mouse is schizophrenic? They can't tell you.
Speaker 1 But it's kind of like that swimming test we told you about earlier. Scientists have categorized behaviors that differentiate between a healthy rat or mouse and, say, a depressed one.
Speaker 1
The depressed rodents don't move around as much. They don't sleep well.
They lose weight. Their fur gets kind of ratty.
They're not so motivated to do tasks that will get them food rewards.
Speaker 1 They kind of sound like depressed people, frankly.
Speaker 3 But of course, mice that seem to be depressed aren't exactly like depressed people, and treatments that work in mice don't always work in people.
Speaker 13 So, a lot of studies have looked at interventions and specific strains of probiotica, treating the animals with it and seeing great results in terms of improvement in anxiety and depression.
Speaker 13 But when they take it to the clinical samples in patients, they just don't see that effect at all.
Speaker 3 But sometimes they do, and some researchers are beginning to do those human studies too. That story after this break.
Speaker 15
With the Spark Cash Plus Card from Capital One, you can earn a limited 2% cash back on every purchase. And you get big purchasing power.
So your business can spend more and earn more.
Speaker 15 Stephen, Brandon, and Bruno, the business owners of SandCloud, reinvested their 2% cash back to help build their retail presence.
Speaker 2 Now, that's serious business.
Speaker 4 What could the Spark Cash Plus Card from Capital One do for your business?
Speaker 6 Capital One, what's in your wallet?
Speaker 15 Find out more at capital1.com slash sparkcash plus. Terms apply.
Speaker 16 You're basking on a beach in the Bahamas.
Speaker 3 Now you're journeying through the jade forests of Japan.
Speaker 7 Now you're there for your alma mater's epic win.
Speaker 3 And now you're awake.
Speaker 1 Womp, womp.
Speaker 3 Which means it was all a dream.
Speaker 7 But with millions of incredible deals on Priceline, those travel dreams can be a reality.
Speaker 16 Download the Priceline app today and you can save up to 60% off hotels and up to 50% off flights.
Speaker 7 So don't just dream about that trip. Book it with Priceline.
Speaker 1 Recently, John decided to take his approach out of the mouse maze and into the wider university.
Speaker 11 We took people that have relatively unhealthy diets and are stress sensitive. Our student population.
Speaker 11 And we decided to put them on a psychobiotic diet for one month or left them on their regular ordinary diet.
Speaker 3 So far, we've been talking about tweaking the microbiome by actually literally putting different microbes into the gut, either by sticking them up the butt in a fecal transplant or eating them like in a supplement.
Speaker 1 For this study, John went about it a different way, because you can also affect the microbes that are living in your gut by changing what you feed them. They eat what we eat.
Speaker 1 A lot of the microbes scientists have studied that create chemicals that seem to help our brains feel happier or calmer, they love the types of foods we're always being told to eat more of, like fermented foods, and vegetables and beans and whole grains that are high in fiber.
Speaker 1 So, when we eat more of those foods, those microbes thrive and multiply, and more microbes means more happy excretions.
Speaker 3 So, that's what John had some of his students eat, which was definitely an improvement on the carbohydrate and alcohol-based diet the control group were undoubtedly surviving on.
Speaker 3 But then, John needed to stress his students to see if the bean-eating ones handled it better.
Speaker 11 We subject them to a public speaking test, so they become quite nervous. In the middle of it, they're told to do a mental arithmetic task they have no idea, so to count back from 2017 in 28.
Speaker 11 And, you know, if they make a mistake, they have to start. We measure a variety of psychological and biological measures.
Speaker 3
Just for the record, the idea of counting back from 2017 in intervals of 28 is not even stressful. It's immobilizing.
I just can't do it. If I was a mouse, I would go straight to float mode.
Speaker 3 Admittedly, I cannot wrangle numbers in my head for the life of me, but still, instant behavioral despair.
Speaker 1 I actually think it sounds kind of fun.
Speaker 1 I keep lots of random numbers in my head, and I think this would be an amusing and somewhat challenging experience, but I can also see how it would start to feel pretty stressful pretty quickly.
Speaker 3 You may be swimming for longer than me, Cynthia, but I bet you'd float eventually.
Speaker 1
Eventually. John and his colleagues didn't put their students in cylinders of water.
Instead, they asked them questions about how stressed they felt.
Speaker 1 And they also did things like look for levels of stress hormones in their blood and saliva. There are biological signals of stress that can be measured.
Speaker 11 And when we looked at all these parameters, what we found was those that had taken the diet that basically was really good for their microbes and really good for their immune system, they had a much greater reduction in this after just one month.
Speaker 1 And in fact, the participants who did the best at following the diet and ate the most fermented foods and other good stuff, they had the most noticeable reduction in stress.
Speaker 3 These are really intriguing results. That said, it was a small study and pretty short.
Speaker 3 And in this study, John didn't measure the impact of his dietary intervention compared to Prozac, for example, so we can't see how eating healthily compares to standard anti-anxiety drugs.
Speaker 1 He also can't prove definitively that it was, in fact, the microbes making a difference.
Speaker 1 Weirdly, the populations and proportions of microbes living in the student guts didn't change dramatically in that month, but some of the fats and other chemicals in their poop changed, and those have been linked to what microbes make.
Speaker 1 So, John's theory is what the students were eating was making the existing microbes in their guts happier, but he says more research is needed.
Speaker 3 And in any case, to show that the microbes were actually creating the difference, he'd have to do something like trace the growth of specific populations of microbes in the students' guts and then study exactly which chemicals they were producing in what quantities, and then trace whether those chemicals were reaching the students' brains.
Speaker 3 And that is a tall order.
Speaker 11 Yeah, causality is one of the conundrums, and that's one of the things that we struggle with in the entire field, and it's something that I feel we need to do more on.
Speaker 2 But then there's also biological plausibility, and that's critically important.
Speaker 2 We know that these pathways exist, and it's plausible that these pathways are activated and can connect the microbiota to the brain.
Speaker 3 That second voice, that is Phil Carl. He was the guy shooting people at the start of this episode.
Speaker 3 He's not only a crack shot, he's a nutrition physiologist in the military nutrition division at the Army Research Institute of Environmental Medicine in Natick, Massachusetts.
Speaker 2 You know, so we have these provocative animal studies using fecal microbiota transplants, and we have biological plausibility to go along with that.
Speaker 1 And this idea that scientists have shown there's a logical way this can work in the human body, there is, as Phil says, biological plausibility. It's enough for Phil and for the U.S.
Speaker 1 Army to spend time, effort, and taxpayer dollars to learn more.
Speaker 2 I fully admit, I'm not entirely convinced. You know, how big of an effect we can have on the brain by manipulating the microbiota.
Speaker 2 And that's one of the reasons why I want to do some of the research myself.
Speaker 2 I think there's a possibility, you know, and I think it's an exciting area of research. So we want to show that in our lab to convince ourselves that, yeah, this is true, this does happen.
Speaker 2 Let's continue down this line of research.
Speaker 3 Phil started down this line of research by just trying to understand what eating frontline military rations, these super portable long-life foods called MREs or meals ready to eat, he wanted to know exactly what living on an all-MRE diet would do to your gut lining.
Speaker 2 And we know that intestinal permeability, gut leakiness, can be related to things like declines in cognitive performance.
Speaker 3 This intestinal permeability, this is what Uma was explaining.
Speaker 3 When inflammatory chemicals made by microbes in your gut leak out through your super delicate gut lining and get into your blood, they seem to be linked with inflammation in your brain and depression.
Speaker 2 So we looked at intestinal permeability, gut leakiness in that MRE study. We actually saw that it improved, gut leakiness improved when individuals ate the MRE diet, which was very nice to see.
Speaker 1 And the reason gut leakiness went down is because MREs apparently have more dietary fiber in them than the standard American diet.
Speaker 1 And the theory is that fiber feeds microbes that excrete chemicals that keep the cell lining intact.
Speaker 3 Which is what Phil wanted to test next, whether eating extra fiber could not only help make a soldier's gut less leaky, but in so doing, make them less stressed and more effective at shooting people.
Speaker 1 This is particularly important for soldiers because one thing that can make a gut extra leaky is extra stress.
Speaker 2 We know that military personnel have to deal with all sorts of stress, sources of stress in their day-to-day lives, and especially when they're in deployed environments.
Speaker 2 So we've been looking for ways to kind of help them manage that stress and perform cognitively better when they're under that kind of stress.
Speaker 2 So I thought probiotics, prebiotics, the gut microbiota, gut brain axis would be an interesting way to try to improve that stress response.
Speaker 1
So probiotics are the microbes themselves. You can buy these as pills.
You can buy them as like pumped up yogurt. They're like extra shots of microbes.
Speaker 1 Prebiotics are the foods that microbes eat, like feeding them extra fiber. Phil wants to test both options to see whether they both could help reduce gut leakiness and reduce stress.
Speaker 3 So for this study, Phil is using supplements.
Speaker 3 His probiotics are bifidobacteria and lactobacillus, and then he's also feeding participants a fiber supplement that our bodies can't digest, but those particular bacteria love to eat.
Speaker 1 And then the idea is to stress out the soldiers and see if the prebiotics or the probiotics help reduce that stress and improve their performance on a bunch of tests.
Speaker 2 So what I thought we could do is we could show you what the kind of ruck march looks like.
Speaker 3 Ruck march, for those of you who are not familiar, is Army shorthand for for marching while carrying a heavily loaded rucksack or backpack.
Speaker 3 According to regulations, the maximum amount a soldier should have to carry while marching long distances is a whopping 45%
Speaker 3 of their own body weight, which strikes me as extremely challenging, but is apparently quite a normal thing to have to do in the field.
Speaker 1 One of his colleagues helped Phil put on a black vest that had a bunch of small weighted bricks on both his front and his back. It was about 50 pounds total.
Speaker 2 30% or so on, which is still a lot.
Speaker 3 And then he got on the treadmill for a pretty brisk uphill walk.
Speaker 3 Phil said the goal is to have participants working at about 60% of their maximum aerobic capacity.
Speaker 2 Yep, you can feel it right away.
Speaker 1 Even after only a minute, Phil's breathing got a little heavy. This weighted march is supposed to last for two hours, and Phil has done the whole thing himself.
Speaker 1 He wanted to experience it before he asked anyone else to give it a go.
Speaker 2 By the end of this, you definitely are not in a good mood.
Speaker 2 And then we have the computer testing that we do.
Speaker 2 So you're trying to not think about the pain on your shoulders, trying not to fall off the treadmill, and trying to do the cognitive test to the best of your ability.
Speaker 2 It really is a challenge and it's aggravating, but that's part of the point.
Speaker 3 Computer testing that Phil mentioned is a couple of different things. One piece is just asking participants about their mood and how hard they feel like they're working.
Speaker 3 And the other piece is a simple matching task. You have to hit a black button when you see a black target and a white button when you see a white one.
Speaker 2 Yeah, so I'm just responding to different pictures that appear on the screen,
Speaker 2 trying to hit the right key that corresponds to the right picture,
Speaker 2 which when you're not doing anything is fairly straightforward.
Speaker 2
And even right now, it's not too hard. But once you can't take your mind off of the pain in your shoulders, it becomes a lot harder.
Or once you're ready to be done with walking for two hours,
Speaker 2 a little bit harder.
Speaker 1 And if this all doesn't sound stressful enough, study participants also have a catheter in their arms the whole time, so Phil and his team can draw blood at regular intervals.
Speaker 1 That way, they can measure things like stress hormones and chemicals that show that someone's gut is a little leaky.
Speaker 3 This kind of tough workout, combined with a cognitive task, is pretty stressful in and of itself. But it's not the only stressful situation that participants in Phil's study will be exposed to.
Speaker 3 It's time to bring in the big guns, literally, after this break.
Speaker 5 Support for this show comes from Pure Leaf Iced Tea. You know that point in the afternoon when you just hit a wall?
Speaker 5 You don't have time for self-care rituals or getting some fresh air, so maybe you grab a beverage to bring you back. But somehow it doesn't do the trick, or it leaves you feeling even worse.
Speaker 5 What you need is a quality break, a tea break.
Speaker 5 And you can do that with Pure Leaf Iced Tea, real brewed tea made in a variety of bold and refreshing flavors with just the right amount of naturally occurring caffeine.
Speaker 5 With a Pure Leaf iced tea in hand, you'll be left feeling refreshed and revitalized with a new motivation to take on what's next.
Speaker 5 The next time you need to hit the reset button, grab a Pure Leaf Iced Tea.
Speaker 3 Time for a tea break?
Speaker 5 Time for a Pure Leaf.
Speaker 17 Avoiding your unfinished home projects because you're not sure where to start? Thumbtack knows homes, so you don't have to.
Speaker 17 Don't know the difference between matte paint finish and satin, or what that clunking sound from your dryer is? With Thumbtack, you don't have to be a home pro.
Speaker 1 You just have to hire one.
Speaker 17 You can hire top-rated pros, see price estimates, and read reviews all on the app. Download today.
Speaker 18 Right here, we're in the dome of the Cognitive Science and Applications team's virtual reality dome, and this is part of the Combat Capabilities Development Command Soldier Center.
Speaker 1
Grace Giles is one of Phil's collaborators on this project. She's a research psychologist and she runs the VR lab.
The lab is dark, and there's a dome you can step into.
Speaker 1 It's like a half dome that kind of surrounds you with the sights and sounds of the scene.
Speaker 18 Here, we're able to bring these basic cognitive tasks into a more realistic scenario, and we think of our virtual reality capability as our bridge between the lab and the field.
Speaker 3 The more realistic scenario, in this case, is where we started the episode. You're walking down a mostly deserted city street, kind of looks like a video game.
Speaker 3
Another soldier is approaching you and you have to decide whether to shoot them or not, i.e. whether they're an enemy or a friend.
And if you get it wrong, you get an electric shock.
Speaker 18 So when they come in here,
Speaker 18 first they will put on a shock belt, which we can show you. And this allows us to induce anticipatory anxiety via the threat of torso shock.
Speaker 18 So it's literally a belt that they'll they'll wear around their waist and we calibrate it to an individual's level of discomfort.
Speaker 1 The first time someone tries this out, the belt just vibrates. After that, they get a small shock, like when it's really dry out and you touch metal and you jump away.
Speaker 1 And then by the end of the experiment, their shock gets just a little shockier.
Speaker 18 So it's meant to be uncomfortable, not painful, and really induce a feeling of anticipatory anxiety in that they're always worried that they're going to make a mistake and get that shock.
Speaker 3 So you're worried about getting shocked and you're trying to figure out who to shoot based on whether they're an enemy or not.
Speaker 3 That already sounds terrible to me, but then Grace ratchets up the stress even more.
Speaker 18 We add a level of complexity by introducing uncertainty in the camouflage patterns.
Speaker 1 Grace pulled up images of friendly camo and enemy camo. Participants have a couple of minutes to study them before they head into the VR dome to start the test.
Speaker 1 They honestly looked almost exactly the same to me until I noticed that the enemy camo has a dark splotch on one thigh and on the abdomen, and friendly camo was more washed out in those areas.
Speaker 18 Phil, do you want to vibrate yourself?
Speaker 3 Phil once again stepped up to the challenge. He put on the shock belt and picked up a Mach M4 assault bike.
Speaker 2 I'm going to call that a foe, so I'm going to shoot.
Speaker 1 I got it right.
Speaker 2 No, so I got a vibration on that one. I didn't make a decision fast enough.
Speaker 1 Each time Phil also has to record how confident he feels about his decision, this is another thing they're measuring.
Speaker 1 They're obviously measuring whether the participants get the decision right, and of course they're doing regular blood and saliva samples.
Speaker 3 Phil sounded relatively chill even when he screwed up. That's probably because he designed the experiment and he's done it before.
Speaker 3 But Grace told us that she and Phil had their first real participant in the lab the day before our visit.
Speaker 3 For his first attempt at the challenge, this guy didn't even get electric shocks, just a little vibration like Phil.
Speaker 1 But he was not so chill.
Speaker 18 I think yesterday's participant felt a little bit more aggravated, even under the vibrate condition, because it is a difficult task because of that level of uncertainty.
Speaker 2 It is frustrating when you're standing up there and you're not getting it right. You're like, why am I not getting it right? Even if it's just on vibration, it just kind of irks you a little bit.
Speaker 2 Like, I thought I had it right this time.
Speaker 1 Eventually, they'll be collecting data from 54 participants, and all those participants will spend about five weeks on the trial.
Speaker 1 During that time, the team will control everything as much as possible so they can really narrow in on the effects of the gut microbes. They tell the volunteers when they can and can't exercise.
Speaker 1 They monitor sleep, they control their diet.
Speaker 2 So, all these factors that we know or think impact the microbiota, we try to control them as much as we can during the studies to eliminate that source of variability.
Speaker 3 Bill expects to be working on this study for another year, and this study is just the start.
Speaker 3 He told us that this first step is in a lab environment, so everything is super controlled, and it's pretty small.
Speaker 2 What we would then do if we see benefit in this study is probably go out into the field for an effectiveness trial where it's a little bit more up to the volunteer, the settings a little bit more unstable.
Speaker 2 We would have more volunteers to get a larger sample size to really show that this works.
Speaker 2 And from there, if we can demonstrate effectiveness in a large field setting, you know, then we start to put the evidence together in order to try to get this type of information and this type of material into specific military recommendations and regulations.
Speaker 1 In other words, it's going to be a long time before this new field of manipulating gut microbes to improve soldiers' mental health, make them less anxious in the field, help them make better decisions, until it's ready for prime time.
Speaker 1 The same is true for the rest of us.
Speaker 1 The effects seem to be real, but scientists need to go bigger to see what happens in the real world when people might have different sleep patterns and maybe they're exercising different amounts.
Speaker 1 They just have totally different lives and environments.
Speaker 3 And researchers know know that those things, exercise and sleep and your home environment, those things can all affect your brain without any need for your gut microbes to be involved, and they can also affect your gut microbes.
Speaker 3 All of these things can happen and probably are happening at the same time, and understanding the whole picture is a long way off. Researchers are just trying to tease out a tiny bit at a time.
Speaker 1 As we mentioned, another problem is that it's hard to prove that any gut microbe changes are the exact thing that affects brain chemistry.
Speaker 1 We can find out if the microbes have changed, but to know for sure, we'd still have to measure what chemicals they're producing and whether and how many of those chemicals get to the brain.
Speaker 1 And those things are currently really difficult to measure in real time in humans. So proving causality is hard.
Speaker 3 Another thing that makes this question of how to manipulate our gut microbes for a healthy brain difficult is we don't even really know what a healthy gut microbiome looks like.
Speaker 11 So you can go and to your physician and get your blood pressure measured, and they'll see where you are in a range. Your cholesterol measured, see where you are.
Speaker 11 You go in with your microbiome readout, they'll just look at you in despair.
Speaker 13 And oftentimes you see in some patient groups, oh, they have a very diverse microbiome. So, you know, is it good? Is it bad?
Speaker 3 It's very difficult to say exactly what is a healthy gut microbiome.
Speaker 13 There are some specific taxa that are associated with better health outcomes and some of them, you know, which are generally associated with worse health outcomes, but it is a very difficult question.
Speaker 3 Right now, it seems likely that there are different ways to have a healthy gut, combinations of microbes that together do the same thing as other completely different microbes.
Speaker 3 Each of these different gut microbiomes is a completely different ecosystem, which means that if you wanted to design an intervention, say a new mental health therapy that targeted the gut microbiome, then it couldn't just be one size fits all.
Speaker 3 There's already evidence that one person's gut microbial community might not respond to the same foods or bacteria as someone else's would.
Speaker 2 So it takes a lot of work to get to that point of being able to recommend certain doses, certain products for certain people at the right time.
Speaker 2 But I think that's where the research community is headed trying to achieve that goal. So we're certainly far from there yet, but I think at some point we will eventually get there.
Speaker 1 It's just going to take a lot of work, a lot of research volunteers, a lot of funding and a decent amount of time it's true that there's still a lot of research to be done but it's also true that scientists have a pretty strong idea that a happy microbiome can help your brain be happier too and vice versa this is not soft science it's not diagnostic it's not prescriptive but there's enough for us to be eating healthier for our better brain health.
Speaker 10 There's more than enough evidence to say that if we're making the efforts slowly and steadily over time, that we can help the health of our microbiome and therefore our mental health as well.
Speaker 3 That said, not a whole lot of mental health professionals are on the gut microbiome train yet.
Speaker 10 It isn't common. I cannot say that the average psychiatrist is practicing this way, but I will tell you that many are interested.
Speaker 3 Again, there's a way to go to even get the field on board. And ultimately, most researchers think that this will be something that people prescribe in combination with therapy or drugs or both.
Speaker 3 It's not necessarily going to be a standalone treatment.
Speaker 1 But the nice thing is it's a pretty low-risk intervention to try.
Speaker 13 But in general, these type of interventions are relatively safe and cheap and with less side effect.
Speaker 3 Eating more fiber or leafy greens or yogurt and kimchi, it's not going to kill you and we do know that it can change your microbiome pretty quickly.
Speaker 1 And that gives agency to people and to patients and you know it allows us to start thinking about our health in a different way and to see if we feed our microbes, could we you know modify our brain and our stress levels and our behavior having agency to improve our stress levels and depression sounds good to me and might sound good to you listeners too but one important note at this point anything you might want to try should really be by changing what you eat not taking pills the probiotics out there aren't regulated they might not be the advertised strain they might not have the same sheer amount of live microbes that they say some are better than others but in general they're considered supplements and as we've already discussed on gastropod there is no real oversight of the supplement market.
Speaker 1 So stick to leafy greens, whole grains, and fermented foods.
Speaker 3 It's all the stuff you've heard before, but now with new mental health benefits.
Speaker 11
So the data we have in our small diet study really says ramp up fiber and fermented foods. That's really good.
Other things that we can say is increase diversity in your diet. Color is fantastic.
Speaker 11 A lot of it contains polyphenols. Now, polyphenol, you know, when I first heard it, I thought it was a 1970s disco queen.
Speaker 11 But polyphenol is really important chemicals that we know get to our microbes and can change our microbes, but also our microbes act on the polyphenols to make certain chemicals as well.
Speaker 3 And those chemicals also seem to be beneficial for our brains. Polyphenols for the win.
Speaker 1 And for these dietary changes to work, they really need to be long-term, like basically forever.
Speaker 1 John started drinking kefir every day, which if you haven't had it, is a really delicious yogurt-like drink.
Speaker 1 These days, I'm personally more likely to have miso, kimchi, or kombucha when it comes to fermented foods.
Speaker 3
I switched to brown rice rather than white. And I think Cynthia would agree.
I'm 100% less of a stress head these days.
Speaker 1 No comment. But one thing is for sure: even though this is still evolving science, we are definitely, as John said, living in a microbial world.
Speaker 13 Okay, now you can drink. I am on a table.
Speaker 1 Thanks this episode to John Crion, Ian Miller, Uma Naidu, Stefani Milan Muller, Phil Carl, Grace Giles, and all their colleagues who also helped us out this episode.
Speaker 1 We have information about their research and books on our website, gastropod.com.
Speaker 3 Thanks also, and as always, to our awesome producer, Claudia Guib, who ventured into the wilds of TikTok for us this episode and came back alive, thank goodness.
Speaker 1 We're heading out to do a bunch of in-person recording together, which we haven't gotten to do as much over the past couple of years.
Speaker 1 And so we'll be back with great brand new episodes for you coming soon. Till then.
Speaker 19 This month on Explain It to Me, we're talking about all things wellness.
Speaker 19 We spend nearly $2 trillion on things that are supposed to make us well: collagen smoothies, and cold plunges, Pilates classes, and fitness trackers. But what does it actually mean to be well?
Speaker 19 Why do we want that so badly? And is all this money really making us healthier and happier? That's this month on Explain It To Me, presented by Pureleaf.
Speaker 20 support for this show comes from Capital One. With the VentureX Business Card from Capital One, you earn unlimited double miles on every purchase.
Speaker 20
Plus, the VentureX Business Card has no preset spending limit, so your purchasing power can adapt to meet your business needs. Capital One.
What's in your wallet?